Overview
Cancer of the cervix is second only to breast cancer as the most common type of cancer found in women worldwide. It affects an estimated 500,000 women each year. In the United States and other developed countries, the rates of cervical cancer are much lower; in fact, according to the National Cervical Cancer Coalition, more than 80 percent of all cases of cervical cancer occur in developing countries.
The American Cancer Society estimates that about 12,170 cases of invasive cervical cancer will be diagnosed in the United States in 2012, and about 4,220 women will die from the disease.
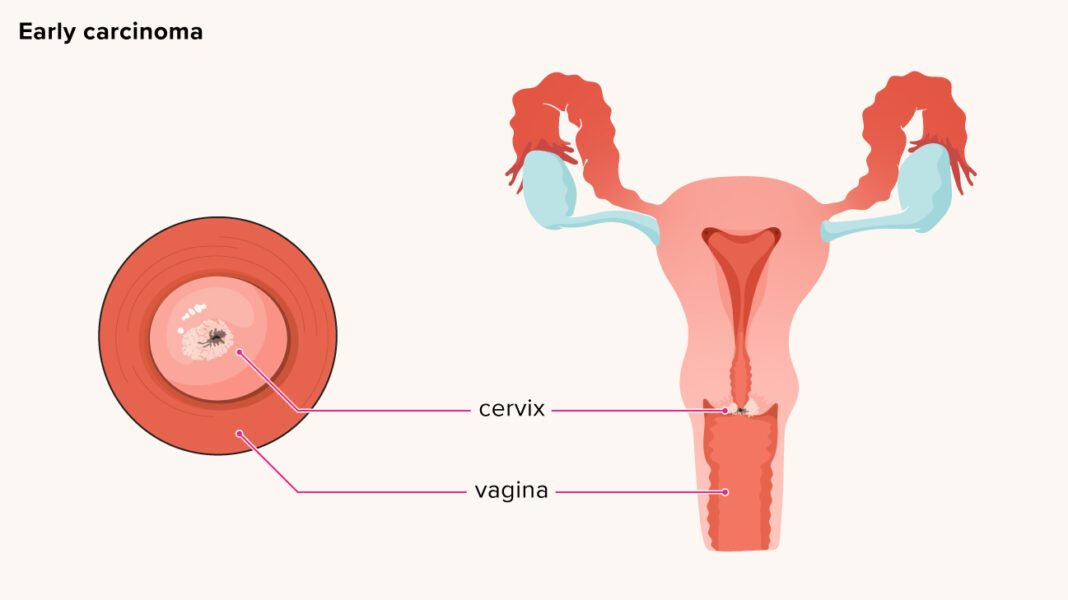
Cervical cancer is a disease in which cancer cells develop in the tissues of the cervix. The cervix, the lower part of the uterus which protrudes into the vagina, connects the body of the uterus to the vagina. Nearly all cases of cervical cancer can be linked to the human papillomavirus, or HPV, a sexually transmitted virus.
Treatment
To plan your treatment, your health care professional needs to know the stage of the disease. The following stages are used for cervical cancer:
- Stage 0 or carcinoma in situ. This is very early cancer. The abnormal cells are found only in the first layer of cells of the lining of the cervix and do not invade the deeper tissues of the cervix.
- Stage I cancer involves the cervix but has not spread.
- Stage IA indicates a very small amount of cancer that is only visible under a microscope and is found in the deeper tissues of the cervix.
- Stage IB indicates a larger amount of cancer is found in the tissues of the cervix that can usually be seen without a microscope.
- Stage II cancer has spread to nearby areas but is still inside the pelvic area.
- Stage IIA cancer has not spread into the tissues next to the cervix, called the parametria. The cancer may have spread to the upper part of the vagina.
- Stage IIB cancer has spread to the tissue around the cervix.
- Stage III cancer has spread throughout the pelvic area. Cancer cells may have spread to the lower part of the vagina. The cells also may have spread to block the tubes that connect the kidneys to the bladder (the ureters).
- Stage IV cancer has spread to other parts of the body.
- Stage IVA cancer has spread to the bladder or rectum (organs close to the cervix).
- Stage IVB cancer has spread to other organs such as the lungs.
The best treatment plans for cervical cancer take into account several factors: the location of abnormal cells, the results of colposcopy, your age and whether you want to have children in the future. Basically, treatment involves destroying or removing the abnormal cells. Three basic approaches are used alone or in various combinations:
Surgery is used to remove the cancer. Various surgical techniques may be used, including:
- excision (cutting out the abnormal cells)
- electrocautery (electric current is passed through a metal rod that touches, vaporizes and destroys abnormal cells)
- cryosurgery (abnormal cells are frozen with nitrous oxide)
- laser vaporization (precise destruction of the small areas of abnormal cells)
- conization (a biopsy used as a treatment)
- simple hysterectomy (removal of the cervix and uterus)
- radical hysterectomy (removal of cervix, upper vagina, uterus and ligaments that support them)
Radiation therapy (using high-dose X-rays or other high-energy rays to kill cancer cells) is used to treat both early and advanced-stage diseases. Sometimes your health care professional will use it alone or in combination with surgery. A common way to receive radiation is externally, just like an X-ray. Another procedure, called brachytherapy, involves having the radioactive source placed inside your body; it continues to emit energy for a specific period of time. In most stages of cervical cancer, radiation should be used with chemotherapy.
Chemotherapy is the use of drugs to kill cancer cells. Chemotherapy may be taken by pill or infused into the body with a needle inserted into a vein. Chemotherapy is called a systemic treatment because the drugs enter the bloodstream, travel through the body and can kill cancer cells outside the cervix. Combination chemotherapy is constantly evolving, with the goal of improving response to treatment. Chemotherapy with platinum can also make radiation more effective, depending on the stage of the cancer.
Based on the stage of your cancer, treatment regimens usually include the following:
- Stage 0 cervical cancer is sometimes called carcinoma in situ. Treatment may be one of the following: conization; laser surgery; loop electrocautery excision procedure (LEEP); cryosurgery; and surgery to remove the cancerous area, cervix, and uterus (total abdominal or vaginal hysterectomy) for women who cannot or do not want to have children. The precancerous changes or the stage 0 cancer can recur in the cervix, vagina or, rarely, the anus, so close follow-up is very important.
- Stage I cervical cancer treatments depend on how deep the tumor cells have invaded the normal tissue.
- Stage IA cancer is divided into stage 1A1 and stage 1A2.
- For stage 1A1, there are a few options. If you still want to be able to have children, your doctor will remove the cancer with a cone biopsy and then closely follow you to see if the cancer returns. If you are through having children or the cone biopsy doesn’t remove all the cancer, your doctor may remove your uterus (simple hysterectomy). If the cancer has invaded your lymph nodes or blood vessels, treatment will involve a radical hysterectomy and removal of the pelvic lymph nodes. If you still want to have children, you may be able to have a radical trachelectomy (surgery to remove the cervix and pelvic lymph nodes) instead of a radical hysterectomy.
- Stage 1A2 involves three treatment options: radical hysterectomy and removal of lymph nodes in the pelvis; brachytherapy with or without external beam radiation; or, if you still want to have children, radical trachelectomy combined with removal of pelvic lymph nodes.If the cancer has spread to the parametria or to any lymph nodes, your doctor will recommend radiation therapy and possibly chemotherapy. If the pathology report reveals that some of the cancer may have been left behind, you may be treated with pelvic radiation combined with chemotherapy and possibly, brachytherapy.
- Stage IB cancer is divided into stage 1B1 and 1B2.
- For pelvic stage 1B1, treatment may involve radical hysterectomy and removal of lymph nodes or para-aortic lymph nodes (lymph nodes higher up in the abdomen), possibly combined with radiation therapy and/or chemotherapy; high dose internal and external radiation; or, if you still want to be able to have children, radical trachelectomy combined with the removal of pelvic and some para-aortic lymph nodes.
- For stage 1B2, the standard treatment is chemotherapy and radiation therapy to the pelvis combined with brachytherapy. In some cases, treatment may involve a radical hysterectomy combined with removal of pelvic and some para-aortic lymph nodes. If your doctor finds cancer in the removed lymph nodes, he or she may recommend radiation therapy after surgery, possibly with chemotherapy as well. And some doctors recommend starting with a combination of radiation and chemotherapy as a first option, followed by a hysterectomy.
- Stage IIA cervical cancer treatment depends on the size of the tumor. If the tumor is larger than four centimeters, treatment may include brachytherapy and external radiation. Treatment may also include chemotherapy with cisplatin. Some doctors recommend removing the uterus after radiation. If the cancer is smaller than four centimeters, treatment may involve a radical hysterectomy and removal of pelvic and some para-aortic lymph nodes. If the removed tissue reveals cancer, treatment will also include a combination of radiation and chemotherapy, possibly with brachytherapy as well.
- For stage IIB cancer, treatment may include internal and external radiation therapy combined with cisplatin chemotherapy and possibly other chemotherapy drugs.
- Stage III and IVA: Most health care professionals combine these two groups in terms of prognosis and treatment. The treatment for these two groups includes combined internal and external radiation therapy with cisplatin chemotherapy. If the cancer has spread to the lymph nodes, especially if it has spread to lymph nodes in the upper part of the abdomen (para-aortic lymph nodes), the cancer may have spread to other areas of the body. Some doctors will check the lymph nodes with surgery, a CT scan or an MRI. If lymph nodes appear enlarged, they will be biopsied. If the para-aortic lymph nodes are indeed cancerous, the doctor may want to do further tests to see if the cancer has spread to other areas of the body.
- Stage IVB cancer treatments often include chemotherapy and/or radiation therapy. Cancer at this stage is not usually considered curable, so treatments are more to relieve symptoms caused by the cancer than to treat the cancer itself.
- Recurrent cervical cancer may require radiation therapy combined with chemotherapy. If the cancer has come back outside of the pelvis, a patient may choose to go into a clinical trial of a new treatment and/or use chemotherapy or radiation therapy to ease symptoms. If the recurrence is limited to the pelvis, radical pelvic surgery may be recommended.
Prevention
Detecting precancerous changes in their earliest stages through regular Pap tests is the best way to prevent cervical cancer. Most women who develop invasive cervical cancer have not had regular Pap tests. Reducing or eliminating risk factors associated with the development of cervical cancer can also help prevent it:
- Don’t smoke cigarettes.
- Use condoms correctly and consistently to protect yourself from sexually transmitted diseases. Note, however, that while condom use will decrease the risk of HPV infection, it can’t prevent it entirely because HPV can infect cells anywhere on the skin in the genital area.
Additionally, the FDA has approved two HPV vaccines, called Gardasil and Cervarix. Gardasil protects women against four HPV types—the two most common high-risk (cancer-causing) types of HPV, strains 16 and 18, and also the two most common low-risk types of HPV, 6 and 11, which cause 90 percent of genital warts. Cervarix protects against HPV 16 and 18. Both vaccines should be given before an infection occurs, ideally, before a girl becomes sexually active. Gardasil is approved for girls as young as nine and is routinely recommended for girls 11 and 12 years of age. It may also be given to women ages 13 to 26 who did not receive it when they were younger, as well as males ages nine to 26. Cervarix is approved for use in girls and women ages nine through 25. If a woman is already infected with one of the four HPV types in one of the vaccines, the vaccine will not work against that particular HPV type. (It will still work against the remaining types she has not yet been exposed to.)
Clinical trials have shown that both Gardasil and Cervarix are safe and 100 percent effective in preventing HPV strains 16 and 18, which cause 70 percent of cervical cancers. Gardasil is also 99 percent effective in preventing HPV strains 6 and 11, which cause about 90 percent of genital wart cases. Both vaccines are given in three injections over six months.
Although Gardasil and Cervarix prevent two of the most serious high-risk HPV strains, these vaccines don’t protect against all of them so the FDA recommends choosing one of them as a complement to safe sex practices and regular Pap tests.
HPV screening of women ages 30 and over is also an important part of preventing potential complications of cervical cancer. The easiest way to screen for HPV is with the HPV test which checks for the virus itself. The Pap test can identify cervical cancer in its earliest stage but can also find abnormal precancerous cells and signs of an active HPV infection.
In conjunction with the Pap test, the HPV test can be used in women over age 30 to help detect HPV infection. Because it specifically tests for the types of HPV that are most likely to cause cervical cancer, when combined with a Pap test in women of this age group, the HPV test is better at identifying women at risk for developing cervical cancer than the Pap test alone.
The American Cancer Society (ACS) and the U.S. Preventive Services Task Force (USPSTF) recommend the following guidelines for early detection and prevention of cervical cancer:
- All women should begin screening at age 21.
- Women ages 21 to 29 should have a Pap test every three years. They should not have an HPV test unless it is needed because of an abnormal Pap test result.
- Women ages 30 to 65 should have both a Pap test and an HPV test every five years or a Pap test alone every three years. (The ACS prefers the two tests together every five years but says either method is acceptable; the USPSTF recommends either schedule.)
- Women over age 65 who have been screened previously with normal results and are not at high risk for cervical cancer should stop getting screened. Women with cervical precancer should continue to be screened.
- Women who have had a total hysterectomy, with removal of their uterus and cervix, and have no history of cervical cancer or precancer should not be screened.
- Women who have received the HPV vaccine should still follow the screening guidelines for their age group.
- Women who are at high risk for cervical cancer, such as women with a family history of the disease, a history of treatment for precancer, DES exposure before birth, chlamydia infection or a weakened immune system (from HIV infection, organ transplant, chronic steroid use or chemotherapy), may need more frequent screenings. Talk to your health care professional about what’s right for you.
The guidelines from the American College of Obstetricians and Gynecologists (ACOG) differ slightly. ACOG recommends that women between the ages of 21 and 29 get Pap tests every two years, and women 30 years of age and older with three consecutive negative Pap tests be tested every three years.
Talk to your health care provider about what is best for you, based on your medical history.
Facts to Know
- The American Cancer Society estimates that in 2012, about 12,170 cases of invasive cervical cancer will be diagnosed in the United States and about 4,220 women will die from the disease.
- The death rate from cervical cancer in African-American women is nearly double that of Caucasian women. Additionally, Hispanic women develop this cancer nearly twice as often as non-Hispanic Caucasian women. The highest rate of cervical cancer is in underdeveloped countries.
- Both incidence and deaths from cervical cancer have declined markedly over the last several decades, due to more frequent detection and subsequent treatment of pre-invasive and cancerous lesions of the cervix from increased Pap screening.
- The five-year survival rate for early invasive cancer of the cervix is 93 percent. The survival rate falls steadily as the cancer spreads to other areas.
- Changes in cervical cells are classified by their degree of abnormality. If your test is abnormal, ask your health care professional to discuss how your abnormalities were described. Many abnormalities return to normal with no treatment, so your health care professional may want to wait and perform another Pap test in several months. Overtreating mild dysplasia can harm the cervix. However, if the Pap results reveal atypical squamous cells of undetermined significance (ASCUS), then HPV testing is routinely done. If no high-risk strains are identified, then no further testing in needed. You should repeat the Pap test in one year. If the Pap reveals ASCUS and the HPV test is positive, a colposcopy will be needed. Colposcopy also is needed if any other more serious changes are shown by the Pap results. Further screening and treatments will depend on the results of the colposcopy. CIN 1 should not be treated, but the Pap will be repeated in 6 to 12 months. For CIN 2-3, further treatment is needed to remove the abnormal cells.
- The primary risk factor for cervical cancer is infection with certain types of the human papillomavirus (HPV). Together, HPV 16 and HPV 18 account for about 70 percent of cervical cancer cases. However, it is important to note that not every HPV infection with high-risk strains is destined to become cervical cancer. Only infections that persist are likely to develop precancerous cell changes if untreated.
- Rates of low-grade squamous intraepithelial lesion (low-grade SIL), usually caused by an active HPV infection, peak in both black and white women between the ages of 25 and 35. However, the number of cases of invasive cervical cancer increases with age, as does the chance of dying from cervical cancer.
- Women who had first sexual intercourse at an early age or who have had many sexual partners or who have partners who have many sexual partners have a higher-than-average risk of developing cervical cancer.
- The majority of cervical cancers develop through a series of gradual, well-defined precancerous lesions. During this usually lengthy process, the abnormal cells can usually be detected by the Pap test and treated.
- Pap tests, like other early detection tests, are not 100 percent accurate. When performed properly, the Pap smear detects a significant majority of cervical cancers—usually in the early stages when the likelihood of a cure is the greatest.